- Home
- Migraine Symptoms
- Auras and Migraines
COMPLETE MAGNESIUM SUPPORT
My Top Choice - Magnesium Breakthrough - The ONLY supplement with all 7 essential magnesium types in one formula. Most only have 1-2 types, leaving you deficient.
Auras and Migraines: Understanding the Symptoms, Risks, and Treatments
Auras and migraines are challenging, to say the least, but are migraine auras dangerous? The answer is nuanced. While most auras are not life-threatening, they do come with certain risks, including a higher likelihood of stroke for some individuals.
During an attack the blood supply to your brain cells is restricted which can lead to cell damage and depending on other risk factors, if your brain tissue is damaged it's called ischemic stroke.
But don't get too alarmed... your risk level is relatively low unless you have one or more other risk factors like family history, obesity or you smoke.
Let’s explore what you need to know about an aura, the symptoms, risks, and effective treatments.
What Is a Migraine Aura?
A migraine aura is a temporary neurological event that typically occurs before or during a migraine attack. It’s like your brain sending a warning signal - sometimes through visual changes, tingling sensations, or difficulty speaking.
The aura phase is the second stage of a migraine, following the prodrome phase (early symptoms like mood swings or food cravings) and preceding the headache phase. Not everyone with migraine experiences an aura, and the symptoms can vary widely.
What Causes Auras?
The leading theory behind auras is cortical spreading depression (CSD). This is a wave of electrical activity that travels across the brain, temporarily disrupting normal neural function. Think of it like a ripple in a pond: it starts small but spreads outward, leaving a temporary period of suppressed brain activity in its wake. This disruption is what creates the symptoms of an aura.
CSD is a wave of electrically excitable neurons and their surrounding cells depolarising. The cells which are normally negatively charged become positively charged. What follows is a period of suppressed neural activity. Neural activity is believed to be the physical basis for thoughts, feelings, and perceptions.
~ Carl Cincinnato, MigrainePal
Types of Auras and Their Symptoms
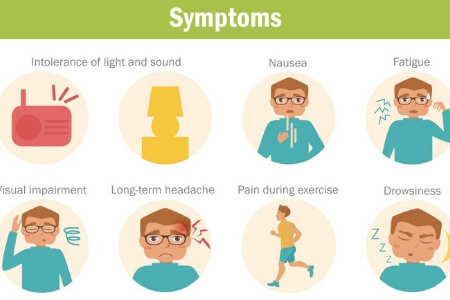
Most people think that an aura is just a visual disturbance. But there are more sensations too. Other types of auras are sensory, language, and motor.
Use these symptoms to help you notice patterns that help you prepare for what’s coming. The symptoms often last between 5 to 60 minutes and can include any combination of these:
1. Visual Auras
- Temporary blind spots or loss of vision
- Wavy, shimmering lines
- Flashing lights or bright spots
- Tunnel vision or distorted shapes
2. Sensory Auras
- Tingling or numbness in the hands, face, or limbs, often on one side of the body
- Strange sensations like vibrating skin
- Feeling overheated or experiencing a "pins and needles" sensation
3. Language Auras
- Difficulty speaking or forming coherent sentences
- Trouble understanding words
- Forgetting words or getting confused
4. Motor Auras
- Temporary muscle weakness
- Paralysis or heaviness on one side of the body
Personal Note:
My own migraine attacks often include a mix of symptoms. For example, my sense of smell and taste are affected, and I sometimes experience a tingling sensation across my face. Symptoms can change over time, so it’s worth noting any new patterns and discussing them with your doctor.

Are Migraine Auras Dangerous?
The short answer? They can be, but the risk is usually low.
The bad news is that if you already get auras and migraines, you are at a higher risk of stroke than people who don't get migraine headaches. The good news is that the increased risk is still relatively low.
Understanding the Risks of Migraine with Aura
1. Restricted Blood Flow
During an aura, blood flow to certain brain regions may decrease, potentially causing cell damage. In severe cases, this could lead to an ischemic stroke, though this is rare.
It is common to find "nonspecific white matter lesions" on MRI's and scans for those of us with migraine aura. But this has not been found to cause cognitive decline in migraine sufferers.
If you get migraine with aura, you're at a higher risk for stroke than others.
Note: absolute level of risk remains relatively low unless you have one or more other risk factors such as smoking, obesity or family history
~ Carl Cincinnato, MigrainePal
2. Stroke Mimicry
An aura can mimic the symptoms of a mini stroke (transient ischemic attack, or TIA), which is a warning sign of a full stroke. Misinterpreting these symptoms as “just another migraine” could delay critical medical care. [1]
Key Differences Between Auras and Strokes
A migraine aura typically has a "slow march" of symptoms that spread gradually and resolve within an hour.
Stroke or TIA symptoms often appear suddenly and are more intense.
The symptoms of TIA that are similar to migraine symptoms:
- Weaknesses, numbness or paralysis of your face, arm or leg on one or both sides of your body.
- Difficulty swallowing, speaking or understanding things.
- Dizziness or loss of balance. You may have an unexplained fall for example.
- Visual disturbance like the loss of vision, or sudden blurry vision in one or both eyes.
- "Headache, usually severe and of abrupt nature or unexplained change in the pattern of headache." [1]
When to Seek Medical Attention
If you experience any of these symptoms, you should see your doctor for further examination. S/he may request a CT scan or MRI to rule out anything serious or any other underlying conditions.
See your doctor immediately if:
- You experience your first aura after age 40.
- Aura symptoms last longer than one hour or are unusually brief (less than 5 minutes).
- You notice new or severe changes in your typical migraine pattern. [1]
WATCH >> THE MIGRAINE WORLD SUMMIT << FOR THE LATEST RESEARCH & PRACTICAL TIPS
Classifications of Migraine with Aura
There are two main categories of migraine as per the International Classification of Headache Disorders (ICHD) and then the 4 aura classifications (there are also subcategories not listed here): [4]
1. Migraine:
1.1 Migraine without aura
1.2 Migraine with aura
Now... let's look at the details for all 4 types of migraine with aura:
1. Migraine with Typical Aura
- Includes visual, sensory, and language symptoms.
- Does not involve motor weakness.
Typical Aura has
- Visual symptoms
- Sensory symptoms
- Language symptoms
Typical Aura does not have
- Motor symptoms
- Brainstem symptoms
- Retinal symptoms
2. Migraine With Brainstem Aura
This type of aura is sometimes called 'Alice in Wonderland Syndrome' due to the very strange body experiences. It is rare, but can occur at any age and is more common in children.
This type of aura may also have visual, sensory and language symptoms, but no motor or retinal symptoms.
You'd have to have 2 of the following symptoms to be diagnosed with this type of aura.
MWB Aura has
- Reduced control over body movements
- Reduced level of consciousness
- Double vision
- Vertigo
- Tinnitus, ringing in the ears
- Slurred speech, inability to speak properly
- Hearing difficulties
MWB Aura does not have
- motor symptoms
- retinal symptoms
Recap: Migraine with Brainstem Aura
- Symptoms include vertigo, tinnitus, double vision, and slurred speech.
- Rare and more common in children.
3. Hemiplegic Migraine
- Involves temporary paralysis or severe weakness on one side of the body.
- Often mistaken for a stroke due to its intensity.
The migraine aura symptoms experienced at the onset of this migraine episode may be temporary numbness, dizziness, or vision changes. So that's visual, sensory and language symptoms. You can see now why diagnosing auras and migraines are tricky.
This type of migraine is most commonly compared to having a stroke as there is temporary paralysis (hemiplegia), along with nerve or sensory changes on one side of the body.
Muscle weakness or motor weakness is most common. Some
sufferers experience this paralysis without the pain phase.
4. Retinal Migraine
- Causes visual disturbances in one eye, such as temporary blindness or flashing lights.
- May or may not accompany headache pain.
I get crushing eye pain with most of my auras and migraines.
Retinal migraine is scary. There is, at the onset, a temporary, partial, or complete loss of vision in one eye, along with a dull pressure or also called a dull ache behind the eye that often spreads to the rest of the head.
The visual aura occurs in one eye only and they may or may not be accompanied by the head pain.
"It may simply involve an aura which may last 5-60 minutes in one eye without head pain from a migraine attack." [1]
Migraine Aura Without Headache
A silent migraine - or migraine with aura without headache - occurs when you experience aura symptoms without the subsequent headache. While it may seem less disruptive, this condition can still be alarming.
For example, if you’re wondering what migraine aura looks like in this context, it often involves visual disturbances like flashing lights or sensory changes such as tingling. Although it’s less common than migraine with headache, it’s equally important to manage and treat.
Treatment and Prevention Strategies for Auras and Migraines
Managing migraine with aura often requires a combination of approaches tailored to your specific triggers and symptoms.
Medications
- Abortive Treatments: Medications like triptans or NSAIDs can stop a migraine attack once it starts.
- Preventive Options: Daily aspirin (300 mg) has shown promise for preventing auras. Beta blockers or anti-epileptic drugs may reduce aura frequency. Always consult your doctor before starting new treatments.
It's essential that you work with your doctor and or specialist to find the right treatment if you get auras and migraines. And ladies... you are more at risk for stroke if you take oral birth control / contraceptives.
Lifestyle Adjustments
- Identify Triggers: Common triggers include stress, dehydration, hormonal changes, and certain foods.
- Maintain a Routine: Regular sleep, meals, and exercise can reduce the frequency of attacks.
- Keep a Journal: Tracking your symptoms helps identify patterns and triggers. Here's my >> Symptom Tracker Journal
Alternative Approaches
- Mindfulness meditation and yoga for stress management.
- Supplements like magnesium or riboflavin (with medical guidance).
FAQs and Practical Advice
Just click on the arrow to show the answer.
What should I do during an aura?
What should I do during an aura?
Answer:
- Find a safe, quiet place to rest.
- Avoid bright lights or loud noises.
- Stay hydrated and try relaxation techniques.
What triggers a migraine aura?
What triggers a migraine aura?
Answer: Triggers vary but often include:
- Stress or anxiety.
- Bright lights or loud noises.
- Hormonal fluctuations.
- Certain foods, such as chocolate or aged cheese.
When should I see a doctor?
When should I see a doctor?
Answer:
- If your aura changes significantly or occur more frequently.
- If you have new symptoms like prolonged weakness or confusion.
While the migraine aura phase can be unsettling - and occasionally risky - it is manageable with the right knowledge and care. Understanding your symptoms is the first step toward effective prevention and treatment. Work closely with your doctor to develop a plan that addresses your needs, and don’t hesitate to seek help for new or severe symptoms.
By staying informed and proactive, you can reduce the impact of migraine on your life and regain control over your health.
Do take care,
Holly
WANT MORE TIPS? Subscribe to my newsletter and follow along on Facebook and Pinterest for all of the latest updates.
MIGRAINE SYMPTOMS Related Articles
How to be more MIGRAINE SAVVY right now...
Auras and Migraines Reference:
1. Cincinnato, C (2015) Migraine with Aura Symptoms. Triggers. Treatment. Available [online] at: https://migrainepal.com/migraine-with-aura/
2. Reviewed by Dr R Senelick (2015) for WedMD Your Guide to Migraine Headaches (Updated August 2019).
3. PubMed.gov (2004) Ophthalmoplegic migraine. Available [online] at: https://www.ncbi.nlm.nih.gov/pubmed/15228891
4. International Headache Society (IHS). ICHD-3. Available [online] at: https://ichd-3.org/1-migraine/
Updated Dec. 1, 2024